Welcome
It is with immense pleasure that we introduce the 2022-23 annual impact report of Health Innovation West Midlands (HIWM) (formerly West Midlands Academic Health Science Network).
As the NHS celebrates its 75th year, 2023 also marks an important milestone for the Health Innovation Network which was established by NHS England 10 years ago to spread innovation at pace and scale. Our purpose remains to lead, catalyse, and drive cooperation, collaboration and productivity between academia, industry, health and care providers and citizens, to accelerate the adoption of innovation to generate continuous improvement in the region’s health and wealth.
As we come to the end of another successful year at Health Innovation West Midlands, we are pleased to share with you significant strides in advancing the quality and accessibility of healthcare services in our communities as a result of the work we have been involved in.
Through our partnerships with our commissioners, colleagues across the Health Innovation Network and our academic, industry, and health and care stakeholders, we have been able to power the development of health technology and services and facilitate the adoption and spread of innovative solutions that have improved patient outcomes and experiences.


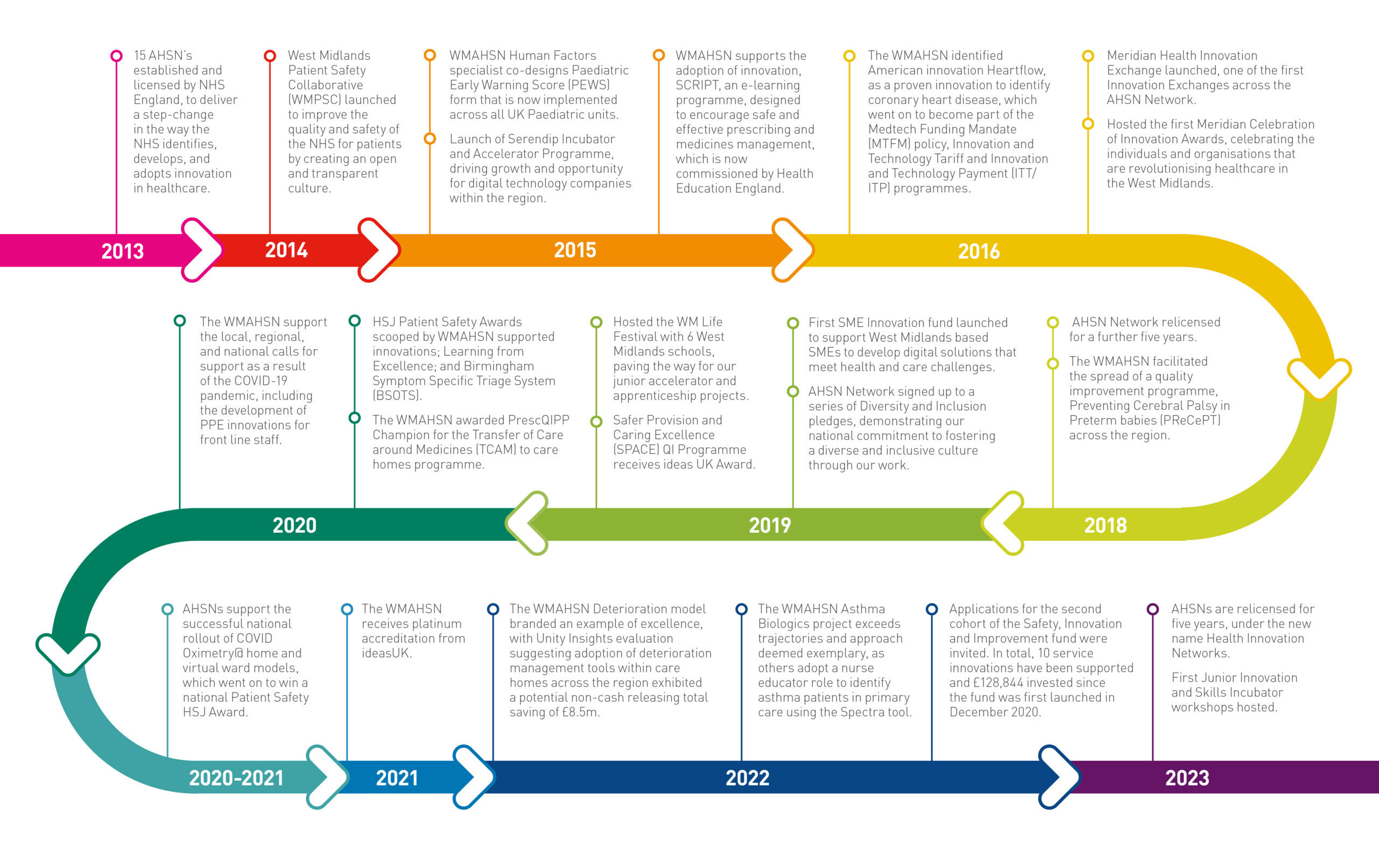
April 2023 marks 10 years since the Health Innovation Network (formerly the AHSN National Network) was established by NHS England to transform the way the NHS identifies, adopts, and spreads promising innovations. During this time, HIWM has undergone significant growth and transformation, and we are excited to share our journey with you through this infographic.
The last decade has witnessed significant changes in the health and care sector, with rapid advances in medical technology driving transformation across the industry and increasing efforts to provide equitable access to care for all. While the COVID-19 pandemic presented significant challenges for the sector, HIWM are proud to have supported the opportunity it presented to spur innovation, collaboration, and resilience in the face of adversity.
As we progress through the timeline, you will see how we have evolved in response to changes in the health and care sector and some of the major milestones and achievements that have shaped our organisation into what it is today.
Case Study Spotlight
Junior Innovation and Skills Incubator

Thopaz+

Managing Deterioration in Care Homes